Welcome to the colon and rectal surgery division at Care New England. Our team of colorectal surgeons and advanced practice clinicians provide comprehensive colorectal care for patients in a safe, caring, and personalized environment.
We care for clinical disorders of the colon, rectum, small bowel, and anus. Our colorectal surgeons specialize in advanced surgical techniques including laparoscopy, robotics, and transanal minimally invasive surgery. We also offer colonoscopies, office-based procedures, surgery, and endoscopy at both Kent Hospital and Women and Infants Hospital.
Our colorectal team is committed to providing the highest quality of cancer care for patients by utilizing a multidisciplinary approach and collaborating with our colleagues in gastroenterology, medical oncology, radiation oncology, pathology, radiology, and genetics to care for our patients.
![]() 455 Toll Gate Road
455 Toll Gate Road
Warwick, RI 02886
![]() 101 Plain Street, 4th Floor
101 Plain Street, 4th Floor
Providence, RI 02903
F: (401) 921-6952
Based on your insurance, you may need a referral from your PCP. Please contact your PCP to request your referral. Contact our office to make an appointment or if you have any questions.
A surgical procedure to remove all (total abdominal colectomy) or part (partial colectomy) of the colon. This is done for many reasons, including large polyps, cancers, inflammatory bowel disease, or diverticular disease. Surgery is typically done through minimally invasive techniques including laparoscopic or robotic surgery.
A surgical procedure to remove all or part of the rectum. Often this procedure involves a temporary or permanent stoma (an opening on the skin where fecal material flows out of the body). Surgery is typically done through minimally invasive techniques including laparoscopic or robotic surgery.
A surgical procedure that involves performing a proctectomy and removal of the anal sphincter resulting in a permanent stoma (an opening on the abdomen where fecal material flows out of the body).
A surgical procedure to remove a segment of the small intestine or to open a narrowed portion of the small intestine.
A minimally invasive approach in which we perform laparoscopic surgery through the anus to remove rectal polyps or early cancers without abdominal incisions.
We offer two approaches for rectal prolapse; the perineal approach (through the anus) called a perineal rectosigmoidectomy, as well an abdominal approach laparoscopic or robotic rectopexy. Your surgeon will discuss with you which approach is best for you.
Anal fistulas may be complex and frustrating for patients. We offer multiple techniques to repair anal fistulas including seton drains, traditional fistulotomy, fistula plugs, endoanal advancement flaps, or ligation of inter-sphincteric fistula tract (LIFT procedure).
A surgical procedure to remove inflamed/bothersome hemorrhoids.
For patients who do not respond to conservative treatment to repair anal fissures, we offer both chemical sphincterotomy (Botox Injection) as well as traditional open or closed lateral internal sphincterotomy.
A surgical procedure in which we implant a sacral nerve stimulator to aid patients with bowel incontinence.
Colorectal cancer is the second leading cause of cancer death in men and women in the United States. Regular screening can detect colorectal cancer early when it is small and has not spread. If found at an early stage, the 5-year survival for colon cancer can be as high as 90%. Screening may prevent colorectal cancer by identifying polyps prior to them turning into cancer.
The American Cancer Society recommends screening for colorectal cancer to begin at age 45 if you are at average risk. If you have a family history of colon cancer or polyps or symptoms you may need to be screened earlier than age 45. Please talk to your doctor about getting screened.
Colorectal cancer starts in the colon or the rectum. It is most commonly seen in older adults but it can happen at any age. It usually begins as small cells in the body begin to grow into small clumps called polyps. The polyps grow over time and may transition and develop into either colon or rectal cancer. Once the cells have turned into cancer cells they can spread locally or travel through the blood and lymphatic system to other areas in the body.
Signs and symptoms of colorectal cancer may include:
Many patients with colorectal cancer have NO symptoms which is why it is important to follow screening guidelines.
There are several factors that can increase your risk of colorectal cancer.
American Society of Colon and Rectal Surgeons Patient Information: https://www.fascrs.org/patients
American Cancer Society: Colon and Rectal Surgery: https://www.cancer.org/cancer/colon-rectal-cancer.html
If you are diagnosed with colorectal cancer, your surgeon will then assess if the cancer has spread either locally or to other areas in your body. They will routinely order “staging” tests which may include abdominal, pelvic, and chest CT scans. For rectal cancer, they may order a rectal MRI or endorectal ultrasound.
Your surgeon will discuss treatment options once the staging of the colorectal cancer has been completed. Treatment may include Surgery, Chemotherapy, and Radiation. Patients with colorectal cancer are discussed at the system-wide gastrointestinal tumor board to discuss the best treatment strategy. The patient’s goals and wishes are taken into account when developing a treatment plan. Our surgeons specialize in minimally invasive techniques for cancer surgery.
Our colorectal surgeons follow Enhanced Recovery After Surgery (ERAS) for all major colon and rectal surgeries. This is part of a “colon bundle” process that has been demonstrated to improve patient outcomes. ERAS allows patients to be active participants in their recovery process. The benefits of ERAS include reduced surgical complications, decreased wound infection, and decreased hospital length of stay. Your colorectal surgeon will provide you with ERAS instructions at your preoperative visit.
Click here to download our ERAS process>>
Following treatment for colorectal cancer, your surgeon will follow national guidelines to assess for recurrence or development of new primary cancer.
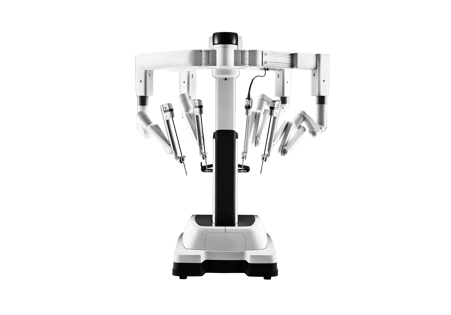
Our colon and rectal surgeons perform surgery using the daVinci Xi robot for a minimally invasive approach to colon and rectal surgery.
The Xi Robot allows the surgeon to perform surgery using state-of-the-art technology to see in 3-D while in high-definition.The surgeon can see better and be even more precise in their surgery, especially when working deep in the pelvis.
Robotic surgeries being performed by the colorectal team include colectomy, proctectomy, rectopexy, and abdominoperineal resection.
Learn from the experts about the various topics related to all things colon and rectal health and wellness.
The question, "why should I get a colonoscopy" is a question I am frequently asked as a colon and rectal surgeon, says Melissa M. Murphy, MD, Executive Chief of Surgery, Care New England Health System...
What are the numbers specific to colorectal cancer affecting the African American population in the United States? In 2019, it was estimated nearly 20,000 African Americans were diagnosed with colorec...
Doctors recommend screening tests to see if you have colon cancer. Several screening tests exist but the gold standard remains a colonoscopy which is both diagnostic and cab be therapeutic. There are ...
Affiliations: Kent Hospital, Women and Infants Hospital, Brigham and Women’s Hospital/Mass General Brigham
Melissa received her medical degree from George Washington University School of Medicine. Prior to enrolling in medical school, she received her Master of Public Health and Master of Medical Science degrees from Boston University. Dr. Murphy completed a research fellowship and general surgery residency at the University of Massachusetts Medical School and completed her fellowship in Colon and Rectal surgery at Brigham and Women’s Hospital and Harvard Medical School. Dr. Murphy is an Assistant Clinical Professor of Medical Science at The Warren Alpert Medical School of Brown University and an Instructor in Surgery at Harvard Medical School.
Colon and Rectal Surgery, CNE
Affiliations: Kent Hospital, Women and Infants Hospital
Lindsay is an experienced advanced practice clinician in the CNE division of Colon and Rectal Surgery. She completed her Bachelor of Science from the University of New England in 2010 followed by her Master of Physician Assistant Studies from the Massachusetts College of Pharmacy and Health Sciences in 2012. Ms. Fink joined Care New England in 2018 and has played an integral part in developing our colorectal program. Her role includes evaluating and treating patients in the clinic setting, first assisting in surgery, and providing inpatient hospital care. Ms. Fink also has prior clinical experience working as a PA in both orthopedic surgery and emergency medicine.
Patients may often feel “embarrassed” to seek a colorectal surgery evaluation and can be scared to have a colonoscopy. We reassure our patients and make sure they feel comfortable and safe. We normalize and acknowledge their concerns. We also provide anesthesia with our colonoscopies to ensure patients have a comfortable experience.
Anorectal surgery can be quite painful due to its location. We typically tell patients that the surgical site may be acutely painful for up to 1 week. In preparation, we provide patients with a nerve block during surgery and inject a long-acting numbing medication surrounding the surgical site. If patients are able to take Tylenol and NSAIDs, we recommend alternating between Tylenol and Ibuprofen (Motrin, Advil) over the counter. If additional pain medication is needed, you will be provided additional medication for the immediate post-operative period. Conservative measures such as warm compresses, soaks in a bathtub, or sitz baths are also encouraged for additional relief.
Copyright © 2025 Care New England Health System